Depending on the nature and severity of an individual patient's condition, the appropriate therapy is determined. For some, simple treatment designed to relax muscles and reduce inflammation is used. For others, more comprehensive diagnostics and treatments are used.
 Successful treatment of TMD once diagnosed, begins with relaxation of mandibular postural (masticatory) muscles. This is achieved with low frequency low amplitude Transcutaneous Electrical Neural Stimulation (TENS). Applied bilaterally to the mandibular division of the Trigeminal Nerve (CN V) through a notch between the coronoid process and condyle of the mandible, all muscles innervated by that nerve are caused to relax. The reference position for the establishment of a therapeutic neuromuscular occlusion is rest position of the mandible.
Successful treatment of TMD once diagnosed, begins with relaxation of mandibular postural (masticatory) muscles. This is achieved with low frequency low amplitude Transcutaneous Electrical Neural Stimulation (TENS). Applied bilaterally to the mandibular division of the Trigeminal Nerve (CN V) through a notch between the coronoid process and condyle of the mandible, all muscles innervated by that nerve are caused to relax. The reference position for the establishment of a therapeutic neuromuscular occlusion is rest position of the mandible.
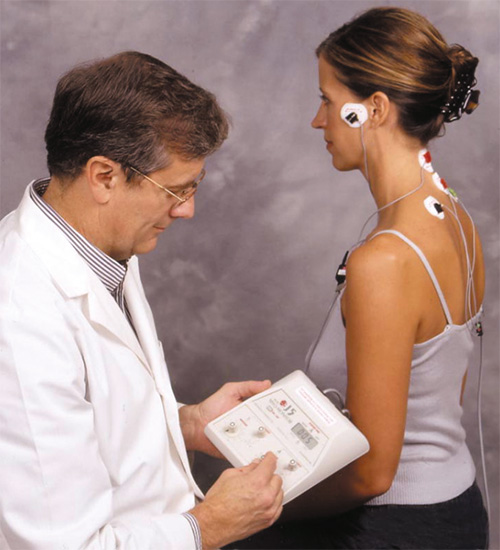
The upper quadrant and cervical muscles can also be simultaneously stimulated to affect muscle relaxation with a second set of TENS leads. This stimulus is discontinued during the later part of the testing protocol when the therapeutic neuromuscular occlusal position is determined and recorded in a bite registration.
DOWNLOAD COMPUTERIZED PATIENT TEST DATA AND PHOTOS
 The three dimensions of rest position are identified through the use of surface electromyography, which monitors resting electrical activity in mandibular elevator muscles (temporalis and masseter) and mandibular depressor muscles (anterior digastric). Rest position is defined as representing the lowest resting activity in the antagonistic muscles. Simultaneous tracking and display on the computer monitor of mandibular position enable the dentist to physically identify the mandible at rest and with that as a reference position, to select a treatment occlusion position along the TENS stimulated arc of jaw movement beginning at-rest position.
The three dimensions of rest position are identified through the use of surface electromyography, which monitors resting electrical activity in mandibular elevator muscles (temporalis and masseter) and mandibular depressor muscles (anterior digastric). Rest position is defined as representing the lowest resting activity in the antagonistic muscles. Simultaneous tracking and display on the computer monitor of mandibular position enable the dentist to physically identify the mandible at rest and with that as a reference position, to select a treatment occlusion position along the TENS stimulated arc of jaw movement beginning at-rest position.
It is not arrived at with the aid of the dentist’s hands, but rather by the TENS stimulated relaxed muscularly controlled jaw movement. This is usually slightly anterior to the natural occlusal position and is actually different in all dimensions. It is called the Neuromuscular Occlusion position
Capturing that position with a bite registration material is the essence of Neuromuscular Dentistry. This bite registration, obtained by TENS stimulation of relaxed muscles, is applicable to the initial phase of TMD treatment involving the use of a removable or fixed orthosis. It is used later if required and desired by the patient in a variety of long term durable treatments. These can involve the further use of orthotic devices full or part-time, restorative dentistry or orthodontics. In some cases, orthognathic surgery may begin the long-term phase of treatment which is followed by other forms of treatment to establish the durable Neuromuscular Occlusion.
Using the information obtained from the computerized recordings of jaw movement and muscle function, and the registration of the new bite position, the doctor constructs a clear or tooth-colored orthotic appliance (orthosis). It is prepared with detailed tooth anatomy to provide a stable biting position. The orthosis, commonly called a "splint," fits over the lower back teeth and passes behind the front teeth, where it can remain invisibly for several months. Worn 24 hours a day, this precise appliance is removed only for cleaning the teeth and the splint. The orthosis permits the jaws to come together in a muscularly healthy position, retraining the muscles to move along a more natural, muscularly oriented pathway into the new occlusion. Patients often report experiencing a significant symptom improvement within a month, while wearing this comfortable appliance.
Following approximately three months of full-time use of the splint, patients are asked to return for a second computerized study of their jaw and associated muscle function. Based on test data, together with the patient's symptom improvement, the outcome of the initial treatment is evaluated and options for additional therapy discussed.
After three to six months wearing the splint, a patient may elect to perpetuate the new healthy biting position either through restoration, shaping of certain teeth, or the use of a removable, durable long-term appliance. Another way to ensure the new bite is through a process called passive eruption. The splint's plastic covering over the rearmost tooth on each side is removed, permitting the last teeth on the top and bottom to erupt naturally as they did when they first entered the mouth. This process, when successful, is repeated by uncovering the next pair of teeth when the rear-most teeth reach the new bite position.
Some patients chose not to wear the orthosis full time, and not to change their natural occlusion. Instead, they may use the orthosis part-time or discontinue usage of the appliance completely unless symptoms reappear. If symptoms reappear, the orthosis can again be used.
A very small percentage of patients with TMD require an evaluation and possible surgical intervention to treat their illness. Except in cases involving severe traumatic injury, which prohibits mandibular function, surgical intervention is usually not indicated as an initial treatment. If conservative treatment, such as splint therapy, has not promoted comfort and proper jaw function, the surgical evaluation may be appropriate.
With the complex interconnection of the temporomandibular joints and the joints of the upper cervical spine and skull, when necessary the neuromuscular dentist may seek collaborative efforts with chiropractors, physical therapists, massage therapists and myofunctional therapists who may dramatically increase the positive outcome in the treatment of TMD disorders. When indicated, the dentist will refer a patient for medical evaluation which could include the specialties of neurology, otolaryngology, ophthalmology, internal medicine, rehabilitation medicine and pain management.